EMS-based MIH programs designed to reduce preventable readmissions may gain traction because of this finding. At MedStar, we’ve seen a significant increase in referrals from our partner hospitals as they derive economic value from reducing readmissions.
Note the reference to staffing issues in in post-acute care settings as a driver of readmissions.
EMS agencies could be a valuable partner for hospitals struggling with readmission rates.
-----------------------
More hospitals to be charged readmissions penalties: CMS
MARI DEVEREAUX
September 15, 2023
https://www.modernhealthcare.com/safety-quality/hospital-readmissions-penalties-increasing-2024-cms
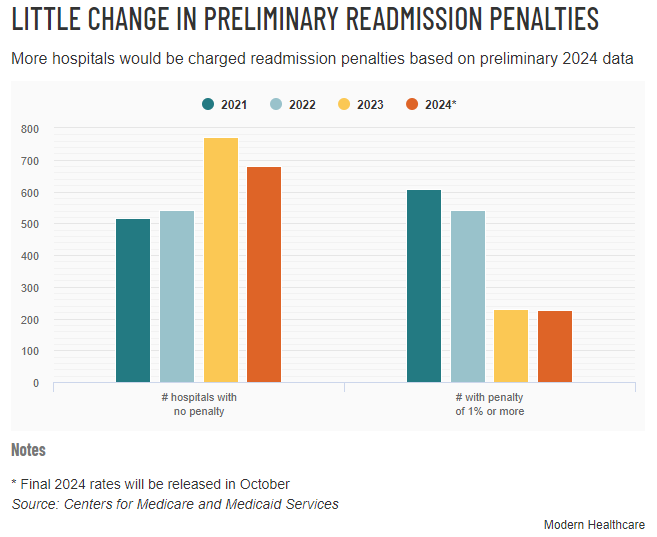
More hospitals will face readmissions penalties in 2024, a departure from the lower rates of reimbursement cuts providers saw last year, according to preliminary data released Thursday.
While the Centers for Medicare and Medicaid Services has resumed use of its pneumonia readmissions measure, which was excluded last year from its Hospital Readmissions Reduction Program, payment adjustments have not returned to pre-pandemic levels.
The hospital readmissions performance period for fiscal year 2024 still excludes data from the first half of 2020, pulling claims from July 2019 to December 2019 and from July 2020 to June 2022. The penalties also exclude data from hospitals with approved extraordinary circumstance exceptions.
“It's probably going to be a messy couple of years,” said Akin Demehin, senior director for quality and patient safety policy at the American Hospital Association. “The ways in which COVID-19 interacts with quality performance on things like readmissions will take time to settle out completely.”
Higher rates of penalties for hospitals likely reflect their hardships during peak months of the pandemic in 2021 and 2022, Demehin said.
For the upcoming year, 70.1% of hospitals will be charged penalties of less than 1% on their readmissions. That compares with 67.1% of hospitals in fiscal 2023.
Meanwhile, 7.5% of hospitals will be charged penalties of 1% or more in fiscal 2024, a percentage virtually unchanged from last year. Another 22.4%of hospitals will not be assessed penalties.
The average penalty for hospitals with the highest proportion of Medicare-Medicaid dual-eligible patients—peer group five—is 0.29%. For hospitals with the lowest number of dual-eligible patients—peer group one—the average penalty is 0.34%. During fiscal year 2023, groups five and one were penalized 0.23% and 0.37%, respectively, on their readmissions.
Before 2020, penalties were on the rise following an increase in measures that are part of the readmissions program.
It is hard to compare readmission rates between periods of the pandemic due to factors like spiking variants affecting hospitals in separate locations at various points in time, said Rick Kes, senior healthcare analyst at RSM.
“You had employment issues in different geographic markets and a pretty substantial increase in traveling nurses, which changed how care was being delivered to patients,” Kes said.
While hospitals have increased their focus on quality and length of patient stay during the past few years, and the acute nature of the pandemic has begun to subside, there are likely still areas of improvement for hospitals to work on, he said.
Understaffing in post-acute care facilities and home health agencies, as well as hospitals’ lack of ability to discharge patients are also problems that contribute to poor readmission rates, Kes said.