Interesting data in the FAIR Health report, but notably lacking is the reasons for out-of-network status of ambulance claims. Likely reasons cited by ambulance agencies have included:
- Lack of interest by insurers to contract with ambulance agencies, citing < 1% of the payer’s spend is on ambulance services and they are focused on providers that represent larger % of their spend.
- Low in-network reimbursement rates offered by insurers, well below the cost-of-service provision.
- The basic in-network model (lower fees in return for higher volume (i.e.: more efficiency) does not work for primarily 911 providers (911 calls represent most out-of-network claims))
- Many public EMS agencies lack the desire to become in-network providers.
You can download the FAIR Health report at the link below – Notable findings are highlighted below.
----------------
Most ambulance rides still out of network
By Maya Goldman and Tina Reed
Sep 13, 2023
https://www.axios.com/newsletters/axios-vitals-4fcd9efd-e475-4636-9f48-149d4b989270.html
Illustration: Sarah Grillo/Axios
Nearly 60% of ground ambulance rides were out of network in 2022, according to an analysis provided first to Axios by FAIR Health.
Why it matters: Patients can't really shop around for an ambulance ride, but they're getting smacked with major medical bills because their emergency transportation is outside of their insurers' network, Tina writes.
- Using its collection of 42 billion private health claims records, FAIR Health found most ground ambulance claims were out of network between 2018 and 2022.
- There was a small decline in out-of-network ambulance rides during that time, from 63.7% in 2018 to 59.4% in 2022.
Our thought bubble: The data indicates that ground ambulances likely remain a large source of surprise bills after Congress dropped them from surprise billing legislation.
What we're watching: A congressional advisory committee last month examined the ground ambulance issue, and it plans to make recommendations in November, per PBS Newshour.
What we're also watching: The internet's favorite physician-comedian Dr. Glaucomflecken's recent take on ambulance bills.
---------------------
Notable excerpts from the FAIR Health report:
- “In addition to being used for transport, ground ambulances can provide on-site treatment, without transporting the patient from the original location to a hospital. Such treatment increased from 2018 to 2020, rising from 1.4 percent to 2.0 percent of all ground ambulance claim lines, but decreased slightly in the following years, dropping to 1.9 percent by 2022.”
- “From 2018 to 2022, response and treatment without transport accounted for a higher percentage of ground ambulance claim lines among individuals aged 19 to 35 than any other age group: between 2.2 and 3.1 percent. By comparison, the age cohort 65 years and older had the lowest percentage.”
More agencies may be finally billing for Treatment in Place (TIP), but the CMS COVID waivers may have impacted this statistic.
Also notable, the data does not include Medicare FFS claims.
Other notable findings in the report:
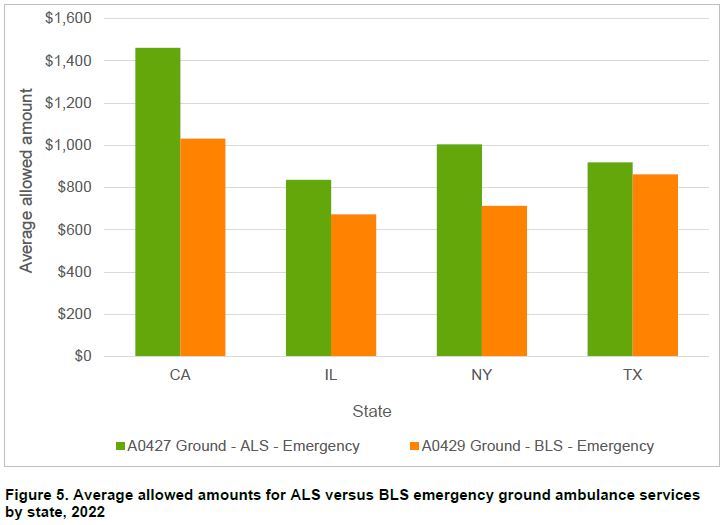
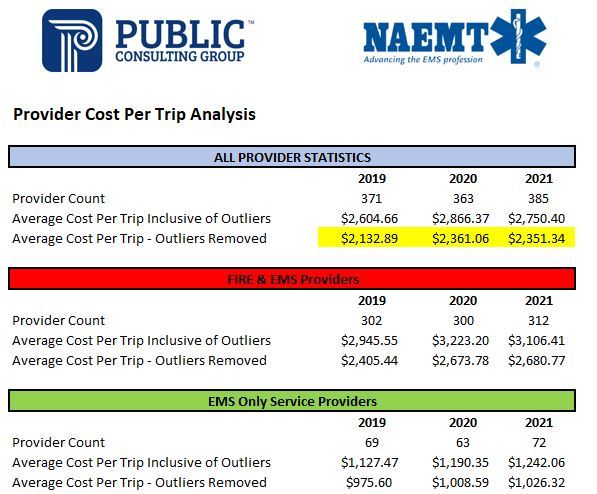
The average allowable fees in these states are below the national average COST of providing service, according to cost report data from the Public Consulting Group.
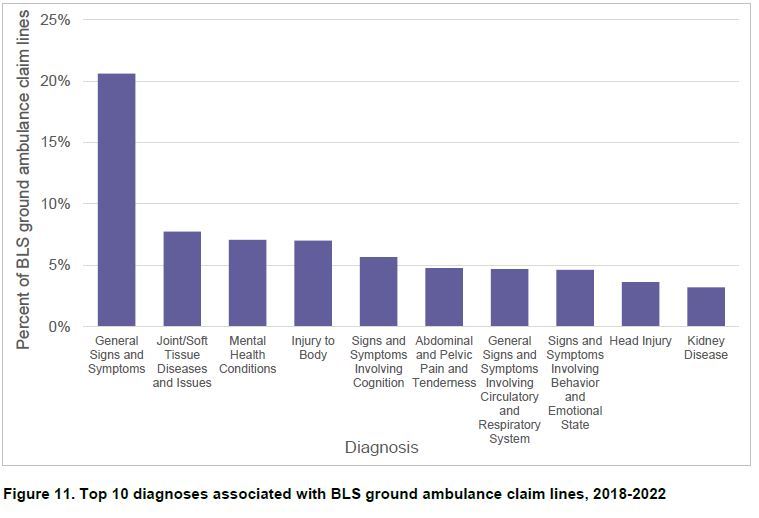
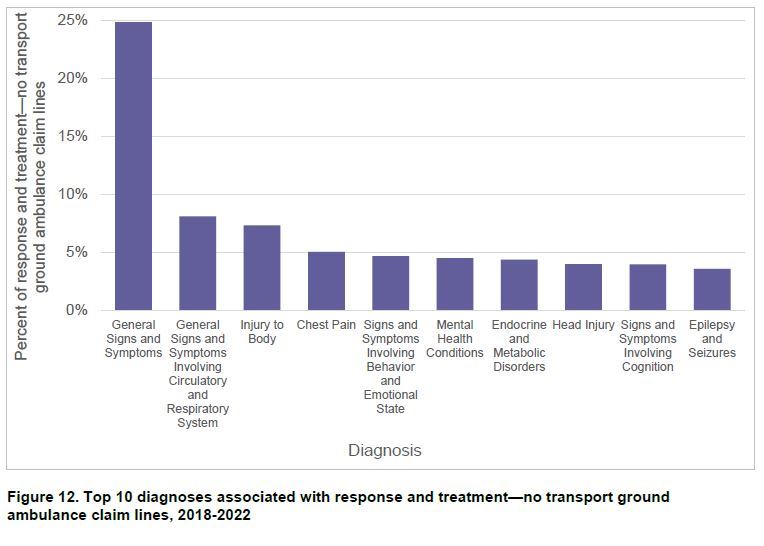
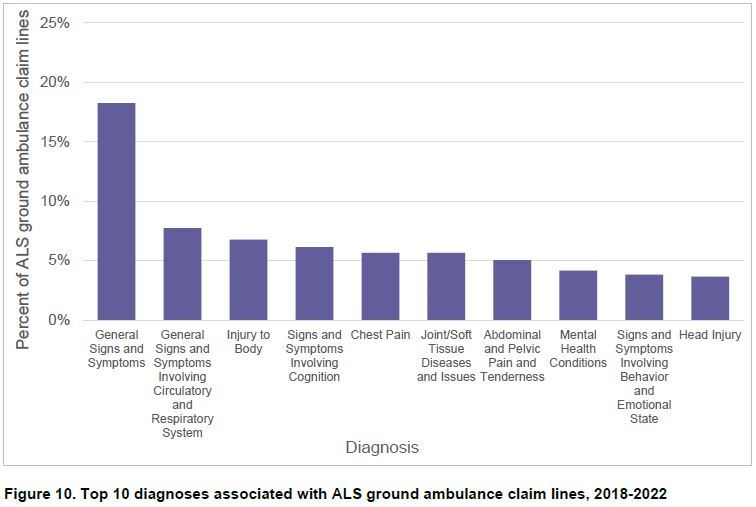
We may need to do a better job of documenting clinical impressions to reduce the number of “General Illness” claims.
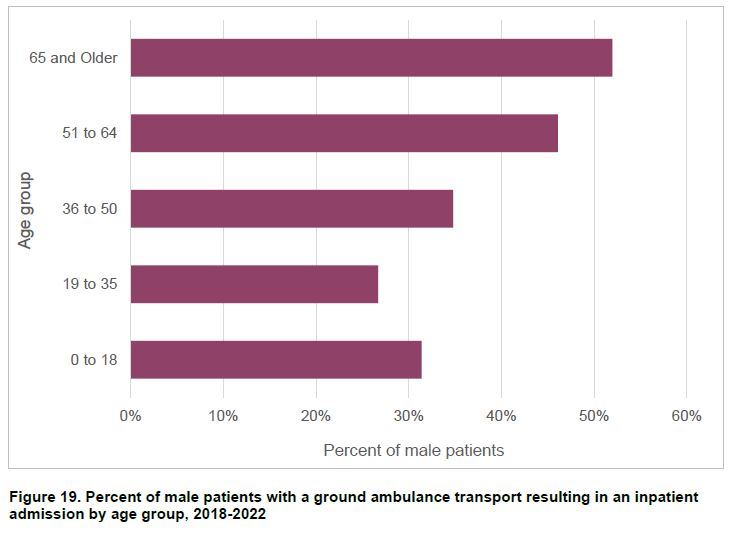
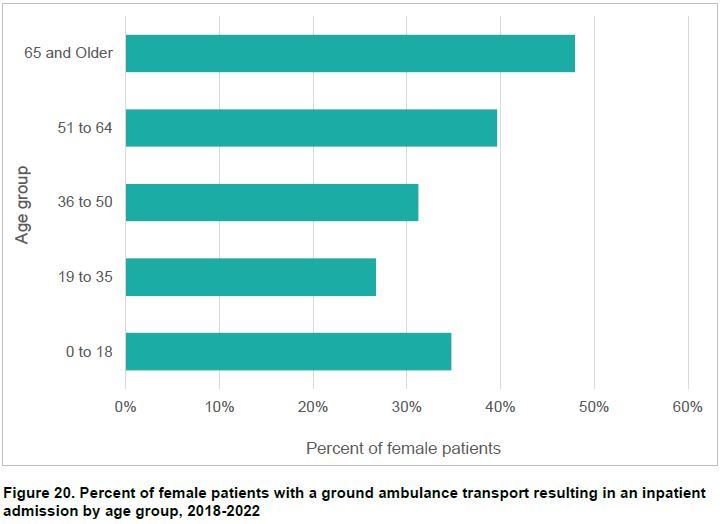
Only about 30% of the patients under 65 transported to the ED by ambulance were admitted to the hospital. Can we do something other than transport to the ED with the other 70% of the patients?